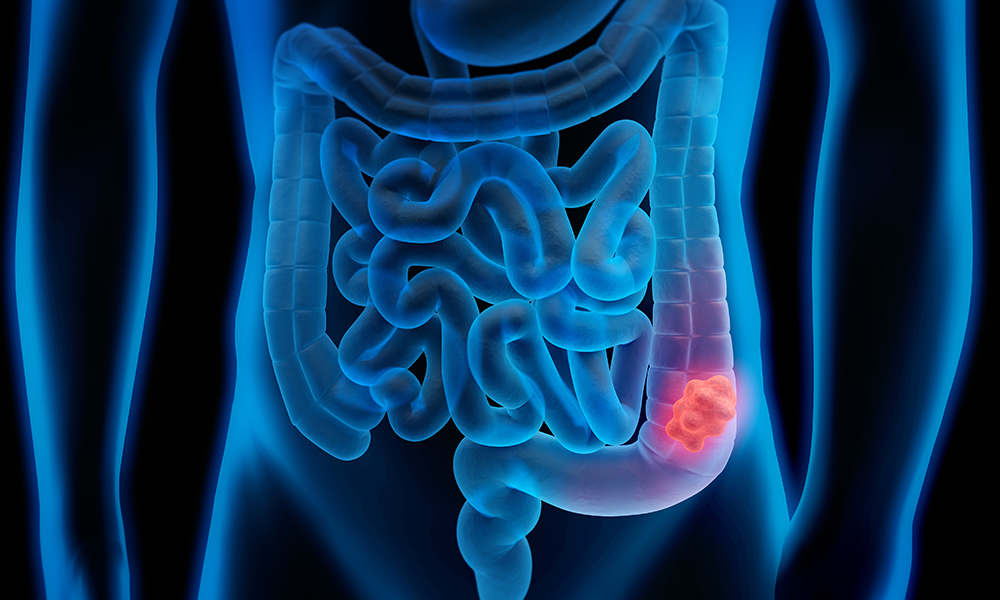
Many digestive conditions share similar symptoms, which can make it challenging for individuals and healthcare providers to differentiate between benign issues and more serious diseases. One common source of confusion lies between Irritable Bowel Syndrome (IBS) and colon cancer.
Both conditions affect the colon and can present with overlapping symptoms, making it crucial to understand when to worry and seek further evaluation. This article explores the similarities and differences between IBS and symptoms of colon cancer, highlighting when medical attention is necessary.
Understanding IBS and Colon Cancer
IBS is a chronic functional gastrointestinal disorder characterized by abdominal discomfort, changes in bowel habits, and bloating. It affects a significant portion of the population and is generally considered non-life-threatening, though it can severely impact quality of life.
Colon cancer, on the other hand, is a malignant growth in the colon or rectum that can be life-threatening if not detected early. Early diagnosis is key to effective treatment and improved outcomes. Recognizing colon cancer warning signs early can save lives, but this is complicated by symptom overlap with IBS.
Common Symptom Overlap
Both IBS and colon cancer can cause symptoms such as abdominal pain, changes in bowel habits (diarrhea, constipation, or alternating patterns), and bloating. These shared symptoms often lead to confusion and delay in diagnosis.
For example, individuals with IBS frequently experience abdominal cramps that improve after bowel movements, while colon cancer patients may report persistent pain unrelated to bowel activity. However, the subtleties between these symptoms can be difficult to discern without medical evaluation.
Key Differences to Notice
Although IBS and colon cancer share some symptoms, certain warning signs should raise suspicion for colon cancer and prompt immediate medical attention.
- Persistent Changes in Bowel Habits: While IBS causes intermittent changes, colon cancer often leads to progressive and persistent alterations, such as narrowing stools or unexplained constipation that worsens over time.
- Blood in Stool: Colon cancer symptoms frequently include blood in stools, either bright red or dark and tarry. While IBS does not cause bleeding, hemorrhoids (common in IBS patients) can, but any blood should be evaluated promptly.
- Unexplained Weight Loss: Significant, unintentional weight loss is uncommon in IBS and may indicate a more serious condition like colon cancer.
- Fatigue and Anemia: Chronic blood loss from colon cancer can lead to anemia, causing fatigue and weakness, symptoms not typically associated with IBS.
When to Worry: Warning Signs
Being vigilant about colon cancer symptoms is vital, especially if you experience any of the following:
- Persistent abdominal pain that does not improve with standard IBS treatments
- Blood in stools or rectal bleeding
- Unexplained weight loss without dietary changes
- A family history of colorectal cancer or polyps
- Fatigue and weakness not explained by other causes
If any of these symptoms occur, it’s essential to consult a healthcare provider promptly for proper evaluation.
Diagnostic Approaches
Distinguishing between IBS and colon cancer requires a combination of medical history, physical examination, and diagnostic tests. Physicians may order stool tests, blood work, and imaging studies, but colonoscopy remains the gold standard for investigating colon cancer symptoms.
Colonoscopy allows direct visualization of the colon lining and the ability to biopsy suspicious areas or remove polyps. Early colonoscopy screening is especially important for individuals with risk factors such as age over 45, family history, or prior history of polyps.
Managing Anxiety While Waiting for Diagnosis
Waiting for diagnostic results can be stressful, especially when symptoms overlap with serious conditions. It’s important to communicate openly with healthcare providers, discuss symptom patterns in detail, and follow their recommendations.
For many, IBS is the more likely diagnosis, but ruling out colon cancer provides reassurance and ensures timely treatment if necessary.
Prevention and Regular Screening
Because early colon cancer symptoms can be subtle or mistaken for IBS, regular screening is essential, particularly for high-risk groups. Colonoscopy screening is recommended starting at age 45 for average-risk individuals, earlier for those with family history or genetic predispositions.
Lifestyle factors such as a balanced diet rich in fiber, regular exercise, limiting alcohol, and avoiding smoking also play a role in reducing colon cancer risk.
Conclusion
Symptom overlap between IBS and colon cancer can cause uncertainty and fear, but understanding key differences helps clarify when to worry. Persistent or worsening symptoms such as blood in stools, unexplained weight loss, and ongoing abdominal pain require prompt medical attention.
By recognizing colon cancer symptoms early and pursuing appropriate diagnostic testing, individuals can improve outcomes significantly. Regular colonoscopy screening and open communication with healthcare providers remain the best strategies for managing this complex symptom overlap.